Long COVID Data and Reports
This webpage has been split into two PDFs for downloading purposes.
Impact of Long COVID Symptoms in Minnesota (PDF)
Minnesotans with Long COVID Symptoms Report Higher Levels of Social Risk Factors (PDF)
On this page:
What is long COVID?
Symptoms reported by Minnesotans
Impact on daily life
COVID-19 vaccination
Insurance coverage
Employment status
Social connectedness
Social needs
What can I do to prevent long COVID?
What should I do if I think I have long COVID?
What is MDH doing to address long COVID?
Impact of Long COVID Symptoms in Minnesota
What is long COVID?
Long COVID refers to infection-associated chronic conditions that can happen after having COVID-19. Many symptoms have been reported, but some of the most common include fatigue, brain fog, extreme tiredness after activity, headaches, muscle pain, change in taste or smell, and shortness of breath. Some people with long COVID have mild to moderate symptoms that gradually get better after a few months. Others have more severe or even debilitating symptoms that can last for several months or years. Findings from the 2023 National Health Interview Survey (NHIS) indicated that 8.4% of adults reported ever having experienced long COVID. This suggests that an estimated 365,000 adults in Minnesota could have experienced symptoms of long COVID.
What did the survey find?
Long COVID symptoms reported by Minnesotans
Over 40% of the survey respondents reported having at least one symptom lasting three months or longer after they had COVID-19. Many experienced symptoms lasting six months or longer. Approximately 1 in 5 respondents had a long-lasting symptom that was severe.
The most common long-lasting symptoms were tiredness, fatigue, shortness of breath, brain fog, and cough.
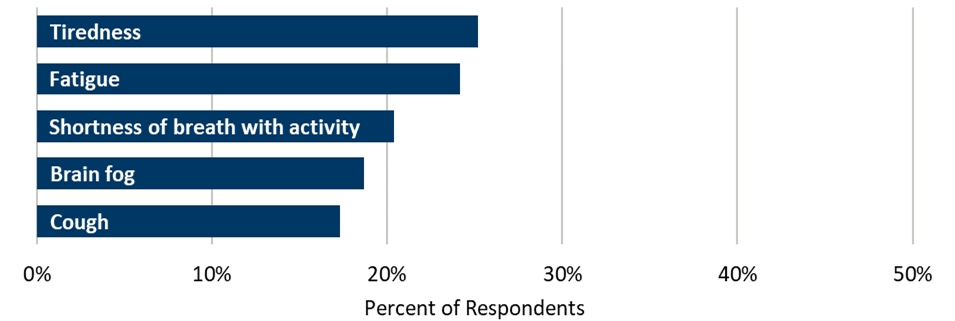
Other commonly reported symptoms included muscle pain, sleep difficulty, headaches, joint pain, and loss of smell or taste. The most common symptoms reported were similar no matter the person’s age, gender, race, or ethnicity.
Nearly half of those who experienced a long-lasting symptom said they had visited a health care provider about a new health issue after their COVID-19 infection, however, only 9% were told by their provider that they may have long COVID. A 2023 poll from the de Beaumont Foundation found that only 7% of physicians felt very confident diagnosing long COVID and only 4% felt very confident treating long COVID.
Long COVID symptoms impact daily life
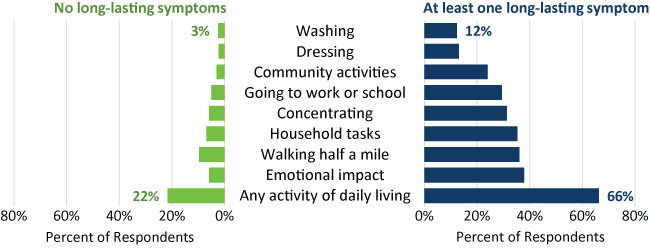
Two-thirds of those with long-lasting symptoms said they had difficulty performing daily activities, such as household tasks or going to work or school.
People with long-lasting symptoms reported more difficulty with activities of daily living.
Fewer long COVID symptoms with more complete COVID-19 vaccination
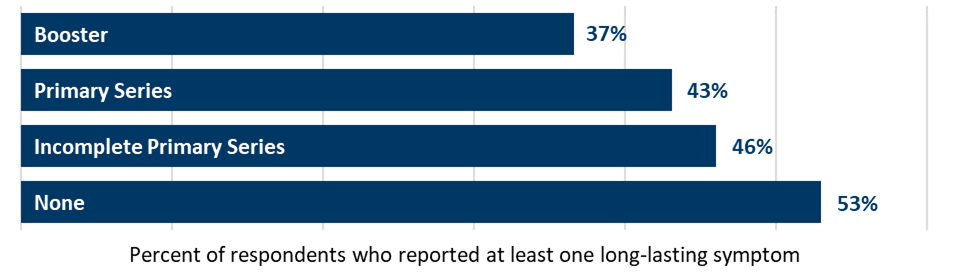
Respondents who completed the primary COVID-19 vaccination series and had received one or more booster vaccines reported 16% fewer long COVID symptoms compared to respondents who were unvaccinated. This is similar to trends seen in recent national studies.
People who were vaccinated at the time of their first infection were less likely to report long-lasting symptoms than unvaccinated respondents.
COVID-19 Vaccination Status
Long COVID and Social Risk Factors
Social determinants of health are the nonmedical factors that influence health. These include, but are not limited to, access to health care, economic stability, food stability, transportation, housing stability, and social support and connections. Social support is important because it can significantly reduce stress, improve mental and physical well-being, and help people live longer, healthier lives.
While this survey cannot tell us what came first – long-lasting symptoms or social risk factors – the results highlight that respondents experiencing long lasting symptoms are also experiencing high levels of health care access needs, economic instability, food insecurity, social isolation, and adverse social connections. Similar findings have been observed nationally. It is critically important to ensure these social risk factors are evaluated and addressed as part of the care, recovery, and support for Minnesotans experiencing long lasting symptoms after a SARS-CoV-2 infection.
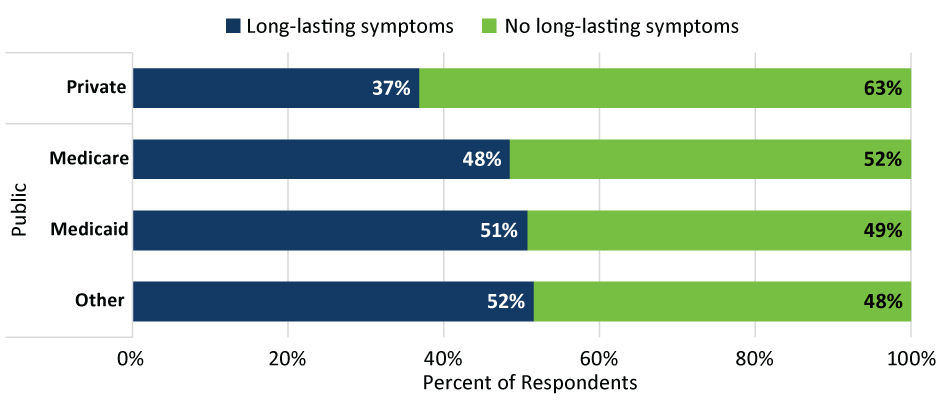
Long COVID symptoms and insurance coverage
Insurance status is often used as a proxy for sociodemographic factors that can affect health care access and status. Overall, 51% of respondents reported private health insurance coverage (such as through an employer), followed by Medicare (18%), Medicaid (16%), and other types of health insurance coverage, which included Veterans Administration (VA) coverage, self-pay and uninsured individuals (15%). About 50% of respondents who had Medicare, Medicaid, or other types of insurance reported long-lasting symptoms, this was even higher among respondents who were uninsured or self-pay (60%). In comparison, only 37% of respondents with private insurance coverage reported long-lasting symptoms.
Respondents with public insurance coverage are more likely to report long-lasting symptoms.
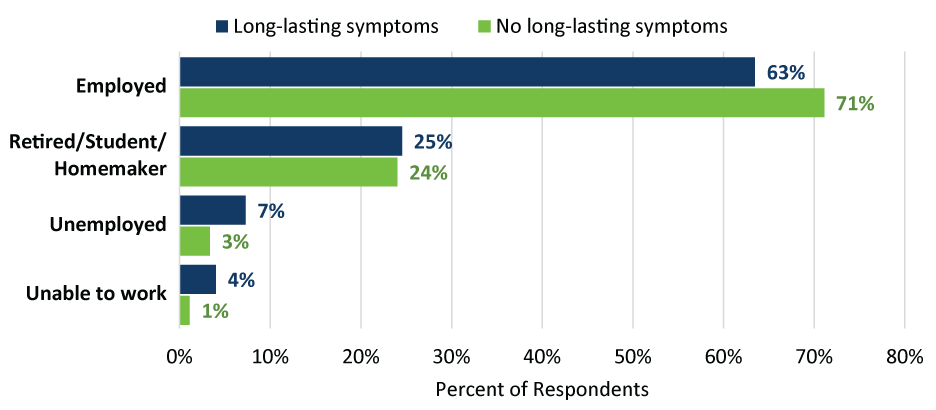
Long COVID symptoms and employment status
Compared to respondents reporting no lasting symptoms, those experiencing long-lasting symptoms were less likely to be employed. Eleven percent of respondents experiencing long-lasting symptoms reported being unemployed or unable to work. This compares to 4% of respondents reporting no long-lasting symptoms.
Respondents with long-lasting symptoms were more likely to be unemployed or unable to work than respondents without symptoms.
Long COVID symptoms and social connectedness
Respondents with long-lasting symptoms were less likely to report neighborhood support and almost four times more likely to report feeling socially isolated and lacking companionship.

Long COVID symptoms and social needs
Difficulty paying for basic needs was three times higher compared to respondents not reporting long-lasting symptoms. Reported food insecurity was three times higher and health care access was more challenging with reports of inability to afford doctor visits or medications also three times higher compared to respondents reporting no lasting symptoms.
Respondents who reported long-lasting symptoms also reported greater economic instability.

What can I do to prevent long COVID?
The best way to prevent long COVID is to avoid getting infected or re-infected with the virus that causes COVID-19. Additional protective measures include:
- Getting an updated COVID-19 vaccine.
- Practicing good hygiene, including washing your hands and covering your cough.
- Taking steps for cleaner air, like opening windows, using filtration, or holding gatherings outside.
- Wearing a mask or keeping physical distance during viral respiratory illness season.
What should I do if I think I have long COVID?
Start by talking with a doctor or health care provider about your symptoms.
- The Centers for Disease Control and Prevention (CDC) offers resources to help you prepare for your appointment: Healthcare Appointment Checklist for Long COVID (PDF).
- Visit Long COVID Resources and Support for more information about medical and social support that may be available to you.
What is MDH doing to address long COVID?
MDH is one of the first state health departments in the country to have a program and staff dedicated to long COVID. Work includes:
- Raising awareness about long COVID and creating informational resources.
- Implementing an ongoing statewide survey to monitor long COVID symptoms and similar conditions in Minnesotans who had COVID-19 or other infections.
- Conducting a statewide study across 12 health systems that provide services to over 90% of Minnesota’s population to recognize and describe patients experiencing long COVID symptoms. This can help improve diagnosis and care practices, especially among underserved patient populations.
- Convening the Long COVID Guiding Council of clinical professionals from 14 organizations, including major health systems, Federally Qualified Health Centers, the Veterans Administration, and the Minnesota Department of Human Services.
- Providing funding to 18 community partner organizations that serve disabled, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), low-income, rural, American Indian, Latine, African American, African immigrant, Asian American, Asian immigrant, and LGBTQ+ communities throughout Minnesota. These organizations reach thousands of individuals disproportionately impacted by the COVID-19 pandemic. They are helping us to understand the impacts of long COVID, raise awareness, and increase access to quality care and support for long COVID and related conditions.
- Serving as national leadership on committees and workgroups for:
- The Centers for Disease Control and Prevention
- The U.S. Department of Health and Human Services Office of Long COVID
- The Agency for Healthcare Research and Quality
- The Association of State and Territorial Health Officials
- The Council for State and Territorial Epidemiologists
- The National Association of Chronic Disease Directors
For more information on our current projects, collaborations, and resources, visit the MDH Long COVID Program webpage.
References
Prevalence of Post–COVID-19 Condition and Activity-Limiting Post–COVID-19 Condition Among Adults | Coronavirus (COVID-19) | JAMA Network. Findings from the 2023 National Health Interview Survey (NHIS).
Poll: Physicians agree Long COVID is a problem but are unprepared to treat it | de Beaumont (PDF). Findings from an online poll conducted by de Beaumont Foundation and Morning Consult among U.S. physicians.
The effect of pre-COVID and post-COVID vaccination on long COVID: A systematic review and meta-analysis | The Journal of Infection. Findings from meta-analysis of 25 observational studies involving over 14 million participants highlight the potential of vaccination to mitigate long COVID’s impact on quality of life.
Our Epidemic of Loneliness and Isolation: The U.S. Surgeon General’s Advisory on the Healing Effects of Social Connection and Community | US Department of Health and Human Services. This advisory calls attention to the importance of social connection for individual health as well as on community-wide metrics of health and well-being, and conversely the significant consequences when social connection is lacking.
Social Determinants of Health and Risk for Long COVID in the U.S. RECOVER-Adult Cohort | Annals of Internal Medicine. Study on those with social risk factors at the time of SARS-CoV-2 infection and their greater risk for subsequent long COVID than those without.
