Methadone
- Fully activates opioid receptors at a controlled, stable level to prevent withdrawal symptoms and reduce cravings (full opioid agonist).
- Can only be provided through federally certified Opioid Treatment Programs (OTPs, also known as methadone clinics).
- Often requires daily in-person visits at the beginning of treatment until take-home doses are permitted.
- Daily (oral) formulations are available to treat OUD.
Buprenorphine
- Partially activates opioid receptors to prevent withdrawal symptoms and reduce cravings (partial opioid agonist).
- Can be prescribed in any clinical setting by any clinician with a standard DEA Schedule III registration.
- Daily (oral) and weekly or monthly (injectable) formulations are available.
Naltrexone
- Completely blocks opioid receptors to prevent opioids from activating them (opioid antagonist).
- Does not relieve withdrawal symptoms or cravings but prevents the effects of opioids if they are used.
- Can be prescribed by any clinician with a license to prescribe medications.
- Requires a period of complete opioid abstinence before starting treatment.
- Daily (oral) and monthly (injectable) formulations are available.
How MOUD works
When opioids like fentanyl enter the brain, they bind to receptors that activate the body’s reward system, slowing down internal organs and providing euphoric effects.
Repeatedly using opioids can result in the development of opioid tolerance. This means more opioids are needed each time to reach the expected effect and prevent the body’s survival system from triggering painful withdrawal symptoms, like nausea, fever, and extreme body aches, that can make it impossible to function in daily life.
For most people with OUD, abstinence alone is not effective because the changes in the brain make withdrawal and cravings extremely difficult to overcome without medication support. MOUD stabilizes these brain receptors, reduces cravings and withdrawal, and allows people to return to daily life while significantly lowering the risk of overdose.
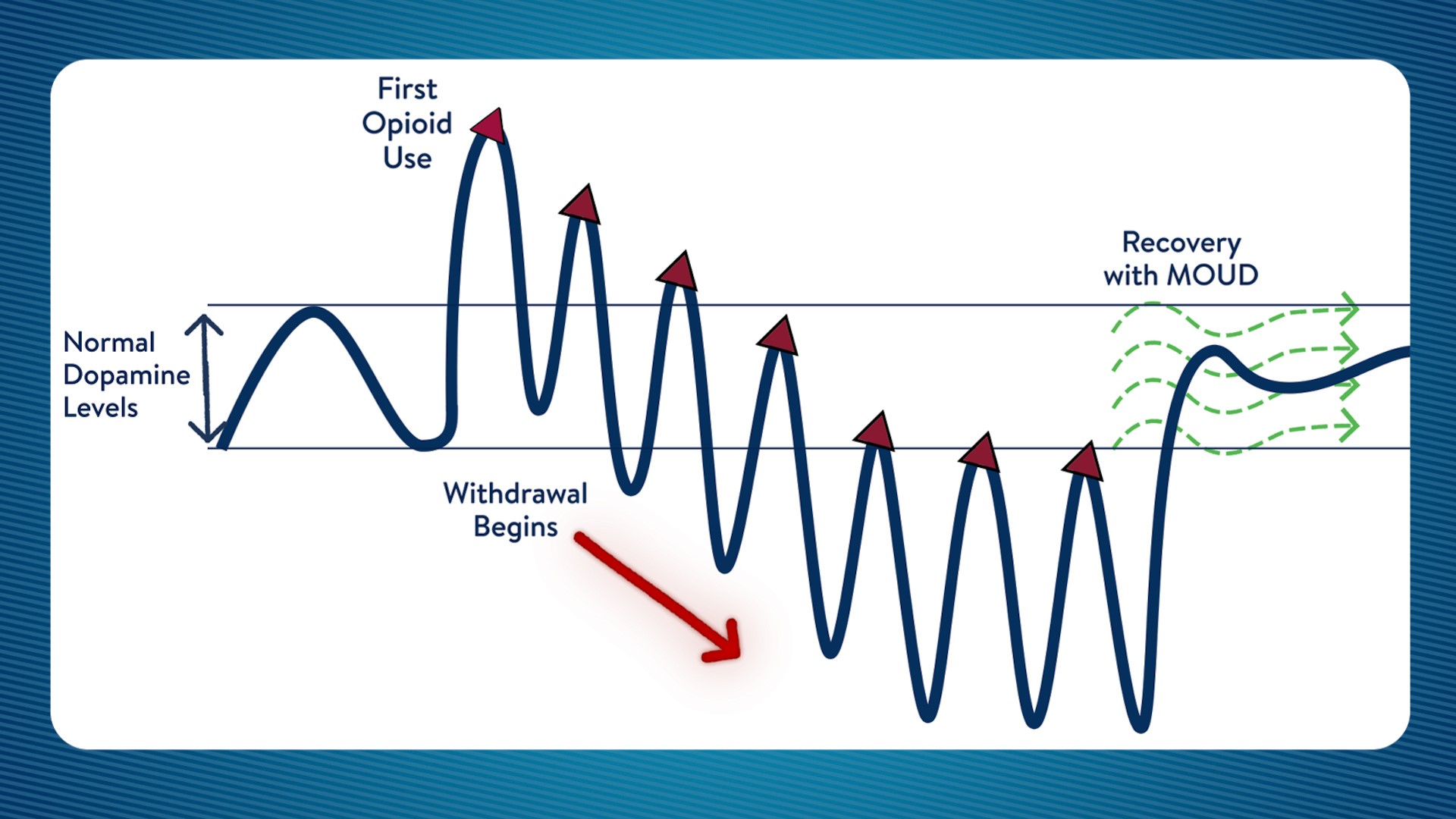
Normal dopamine levels in the brain vary throughout the day. Opioid use raises these levels significantly, until withdrawal symptoms throw this cycle out of balance. With MOUD, patients can get their dopamine levels back into the normal range and focus on recovery.