Annual Summary of Disease Activity:
Disease Control Newsletter (DCN)
Related Topics
Contact Info
Salmonellosis, 2015
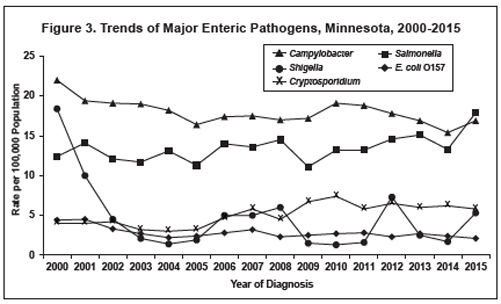
In 2015, 975 culture-confirmed Salmonella cases (17.9 per 100,000 population) were reported (Figure 3). This is a 36% increase from the median annual number of cases reported from 2005 to 2014 (median, 717; range, 578 to 810), and the highest annual case count reported in Minnesota since 1989. The increase was largely due to 200 outbreak-associated cases.
Of the 91 serotypes identified in 2015, 6 serotypes, S. Enteritidis (229), S. Newport (132), S. I 4,[5],12:i:- (88), S. Typhimurium (81), S. Poona (46), and S. Heidelberg (37) accounted for 63% of cases. All but 3 of the S. Poona cases were associated with one large outbreak. Salmonella was isolated from stool in 859 (88%), urine in 62 (6%), and blood in 40 (4%) cases. Other specimen sources included cerebrospinal fluid, paracentesis fluid, bile fluid, abdominal aortic aneurysm, pancreas pseudocyst, eye swab, breast, shoulder tissue, and wound.
Two hundred sixty-four (27%) cases were hospitalized for their infection; the median length of hospital stay was 4 days (range, 1 to 78 days). One culture-confirmed Salmonella case died; a 53 year-old who died of metastatic malignancy 5 days after S. Enteritidis was isolated from a paracentesis fluid specimen.
Of the 887 cases asked about travel, 132 (15%) had traveled internationally during the week prior to their illness onset. There were 3 S. Typhi cases; 2 had traveled or emigrated from India, and 1 did not report any travel. There were 2 S. Paratyphi A cases; 1 had traveled to India, and 1 did not report any travel.
In 2015, culture-independent tests became commercially available for the detection of Salmonella nucleic acid in stool. Two patient specimens that were positive by a culture-independent test conducted at a clinical laboratory were not subsequently culture-confirmed, and therefore did not meet the surveillance case definition for inclusion in MDH case count totals.
Two hundred cases were part of 18 Salmonella outbreaks identified in 2015, including 2 cases that were part of a multi-state outbreak but who were not exposed in Minnesota (no cases were exposed in Minnesota in this outbreak). Twelve of the outbreaks involved foodborne transmission, three person-to-person transmission, one animal contact, and two outbreaks were due to other modes of transmission (laboratory-acquired, and exposure to raw suet). Nine of the outbreaks, including the non-Minnesota outbreak, involved cases in multiple states. The 18 outbreaks resulted in a median of 5 culture-confirmed cases per outbreak (range, 1 to 81 cases).
In January, 2 S. Dublin cases were associated with exposure to beef products sourced from the same Minnesota distributor. The outbreak strain was found in a sample of beef suet (purchased for bird feed) collected from one case’s household.
In January, 1 laboratory-confirmed and 4 probable S. I 4,5,12:b:- var. L(+) Tartrate+ cases were part of a person- to- person outbreak at an in-home daycare.
In March, 4 laboratory-confirmed and 3 probable S. I 4,[5],12:i:- cases were linked to an outbreak at two locations of a Mexican-style chain restaurant. Guacamole was identified as the probable vehicle, but the contaminated ingredient and source were not identified. Also in March, 3 S. Poona cases were acquired via person-to-person transmission among three extended family members in two households. The original source of the index case’s infection was likely reptile contact at another family member’s house. Also in March, 9 S. I 4,[5],12:i:- cases were associated with an outbreak at one location of a fried chicken chain restaurant. Cross-contamination of coleslaw with Salmonella from raw chicken by a food worker during preparation was the most probable cause of the outbreak. Lastly, 2 S. Newport cases were part of a multistate outbreak of 25 cases from 10 states likely associated with Mexican-style cheese. The Minnesota cases both traveled to Mexico and were likely exposed there.
During April through July, 8 S. Enteritidis cases were part of a multistate outbreak of 15 cases in 7 states associated with raw frozen stuffed chicken products. A local and national press release was issued and a recall initiated.
In April, 8 S. Paratyphi B L(+) tartrate+ cases were part of an outbreak at a steak restaurant. Several outbreak cases were also identified in West Virginia. Consumption of the house salad was associated with illness. Due to the number and collinearity of ingredients in the house salad, the implicated ingredient could not be identified epidemiologically. A lack of traceback efforts by external federal partners further prevented identification of the vehicle and source of contamination.
In May, 10 S. Enteritidis cases were part of a multi-state outbreak of 252 cases in 43 states with several Salmonella serotypes (Enteritidis, Hadar, Indiana, Muenchen, and Muenster) associated with live chicken contact. While a common hatchery was not identified, contact with poultry, particularly with young poultry, is a well-known risk factor for Salmonella infections in humans.
During May through July, 5 laboratoryconfirmed S. Enteritidis cases were associated with consumption of raw frozen stuffed chicken products. A local and national press release was issued and a recall initiated. This outbreak was caused by a different brand/ manufacturer and was not associated with the April – July outbreak.
During June through October, 3 laboratory-confirmed and 7 probable S. Agona cases were part of a graduation party outbreak associated with pork prepared from a whole roasted pig. Undercooking and temperature abuse likely contributed to the outbreak.
In June, 4 laboratory-confirmed S. Paratyphi B L(+) tartrate(+) cases were part of a multi-state outbreak of 65 cases in 11 states associated with consumption of sushi products made with raw frozen tuna imported from Indonesia. A local and national press release was issued and a recall initiated.
In August, 7 laboratory-confirmed and 2 probable S. Virchow cases were part of an outbreak at a restaurant. Consumption of lobster guacamole was significantly associated with illness. Cross-contamination and hand hygiene issues were a likely mechanism for cross-contamination of the guacamole from a raw food of animal origin.
During August 2015 through January 2016, 45 laboratory-confirmed and 3 probable S. Poona cases were part of a multi-state outbreak of 907 cases in 40 states linked to garden cucumbers imported from Mexico. Many of the Minnesota cases were exposed at multiple locations of a sandwich chain restaurant and a seafood chain restaurant that received the implicated cucumbers. A local and national press release was issued and a recall initiated.
During August and September, 81 laboratory-confirmed and 34 probable S. Newport cases in Minnesota residents were associated with tomatoes served at multiple Mexican-style chain restaurant locations in Minnesota and Wisconsin. Four S. Newport cases in Wisconsin residents were identified who were also part of the outbreak. Tomatoes were implicated as the outbreak vehicle by an ingredient-specific analytic study, supported by internal product distribution information provided by the corporate restaurant owner. The ultimate source of contamination (i.e., the tomato farm or packing house) was not identified.
During August through November, 5 S. Typhimurium cases were part of a multistate outbreak of 109 cases in 38 states associated with exposure to the ATCC strain of S. Typhimurium in clinic and teaching microbiology laboratories.
In October, 2 laboratory-confirmed and 3 probable S. Typhimurium cases were associated with a person-to-person outbreak at a child care center.
During December 2015 through March 2016, 3 S. Virchow cases were part of a multi-state outbreak of 33 cases in 23 states associated with an organic packaged meal replacement powder. The manufacturer recalled all lots of product with “best by” dates from August 2017 to December 2017. Organic moringa leaf powder was the contaminated ingredient in the product.
- For up to date information see>> Salmonellosis (Salmonella)
- Full issue>> Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health, 2015